Gut Health Assessment Quiz
Key Takeaways
- Knowing how the digestive system works helps you catch issues early.
- Fiber, water, and a balanced microbiome are the core of good gut health.
- Simple gut health tips like regular meals and stress control can transform how you feel.
- Probiotics and prebiotics each have a role - choose the right one for your needs.
- A quick daily checklist keeps your gastrointestinal health on track.
Most people focus on calories, cardio, or skin care, but the real powerhouse behind energy, mood, and immunity is the gut. Gastrointestinal health means the digestive tract functions smoothly, absorbing nutrients while keeping harmful agents out. When it falters, you might feel sluggish, bloated, or irritable without realizing why. This guide walks you through the science, everyday habits, and clear actions you can take right now.
1. What Makes Up the Digestive System?
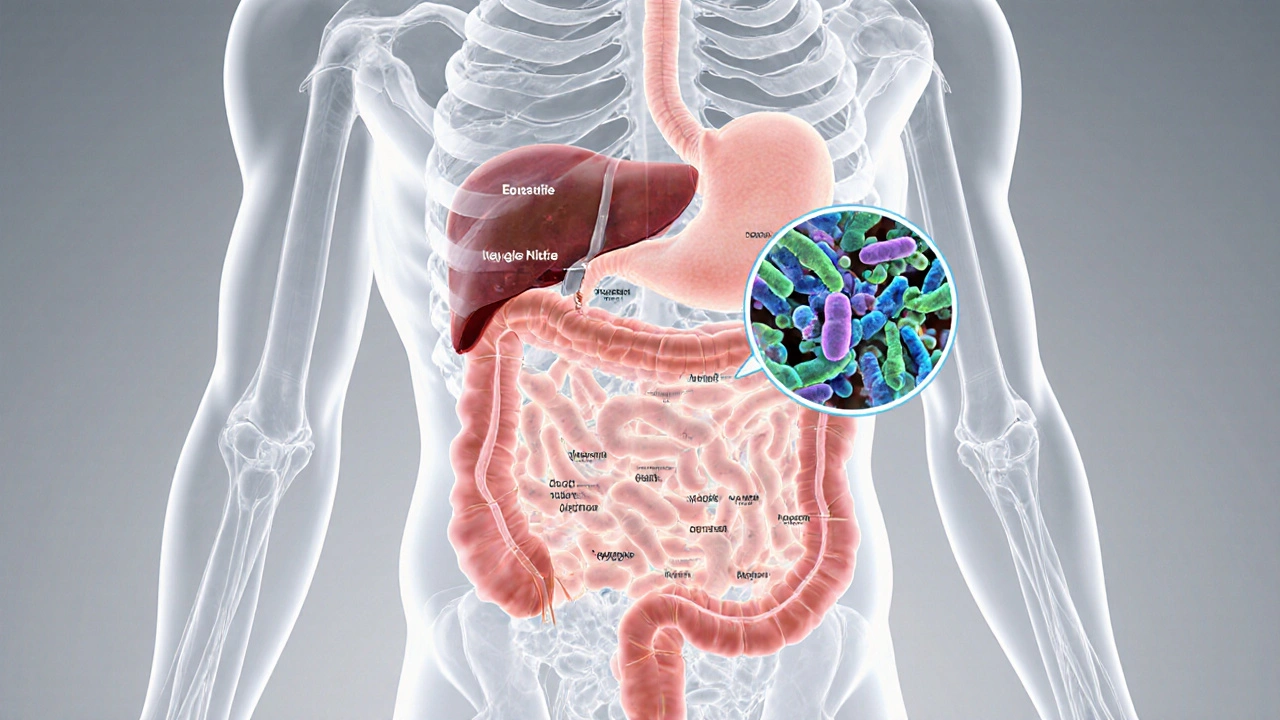
The digestive system includes the mouth, esophagus, stomach, small and large intestines, and accessory organs like the liver and pancreas. Its main jobs are breaking down food, extracting nutrients, and eliminating waste.
A less obvious player is the gut microbiome a community of trillions of bacteria, fungi, and viruses that live in the large intestine. These microbes help digest fiber, produce vitamins, and train the immune system. An imbalance-often called dysbiosis-can trigger bloating, constipation, or even mood swings.
Common conditions you’ll hear about:
- Irritable Bowel Syndrome (IBS) a chronic disorder causing abdominal pain, gas, and irregular bowel movements
- Gastroesophageal Reflux Disease (GERD) heartburn and acid back‑flow from the stomach into the esophagus
- Inflammatory Bowel Disease (IBD) encompasses Crohn’s disease and ulcerative colitis, both involving inflammation of the intestinal lining

2. Lifestyle Foundations for a Happy Gut
Before you reach for supplements, lock in the basics.
Fiber - the Unsung Hero
Fiber is the food that feeds the good bacteria. Aim for 25‑30g per day, split between soluble (oats, apples, beans) and insoluble (whole‑grain breads, nuts, seeds) types. Soluble fiber forms a gel that slows sugar spikes, while insoluble fiber adds bulk to keep things moving.
Hydration
Water helps dissolve nutrients and softens stool. A rule of thumb: drink half your body weight in ounces each day, plus extra if you’re active or live in a hot climate.
Sleep and Stress
Both sleep deprivation and chronic stress disturb the gut‑brain axis, leading to altered motility and microbiome shifts. Aim for 7‑9hours of quality sleep and incorporate stress‑busting habits like deep breathing or short walks.
3. Nutrition Strategies That Really Work
Now let’s talk food and supplements that can tip the balance toward health.
Probiotics vs. Prebiotics
Probiotics are live microorganisms you ingest, while prebiotics are non‑digestible fibers that act as fertilizer for those microbes. Both have merit, but they serve different purposes.
| Feature | Probiotic | Prebiotic |
|---|---|---|
| What it is | Live beneficial bacteria | Fermentable fibers |
| Typical sources | Yogurt, kefir, fermented vegs, supplements | Garlic, onions, bananas, chicory root, whole grains |
| Primary benefit | Replenish specific strains | Feed existing gut microbes |
| Best use case | After antibiotics or acute GI upset | Long‑term maintenance of a diverse microbiome |
If you’ve just finished a course of antibiotics, start with a probiotic that contains Lactobacillusacidophilus and Bifidobacteriumlactis. For everyday maintenance, load up on prebiotic foods-think a handful of berries with your oatmeal or a salad topped with roasted garlic.
Smart Meal Timing
Skipping breakfast can confuse your gut’s natural clock. Aim for three balanced meals plus a snack if you need extra fuel. Try to keep 4‑6hour gaps between meals; this gives the intestine time to empty and reduces fermentation‑related gas.
Specific Nutrients to Watch
- Omega‑3 fatty acids - anti‑inflammatory; found in fatty fish, flaxseeds, walnuts.
- Polyphenols - support beneficial bacteria; present in green tea, berries, dark chocolate.
- Vitamin D - linked to gut barrier health; get sunlight and fortified foods.

4. Red Flags - When to Call a Professional
Most gut complaints improve with diet tweaks, but certain signs warrant a doctor’s opinion.
- Blood in stool or black, tar‑like stools.
- Unexplained weight loss >5% over a month.
- Persistent vomiting, severe abdominal pain, or fever.
- Changes in bowel habits lasting longer than three weeks.
Bring a symptom diary to your appointment. Note what you ate, stress levels, and timing of any discomfort. This data helps clinicians pinpoint conditions like IBD or celiac disease.
5. Your Daily Gut Health Checklist
- Drink a glass of water within 30minutes of waking.
- Eat a fiber‑rich breakfast (e.g., oatmeal with berries and chia seeds).
- Take a probiotic capsule if you’ve been on antibiotics or feel bloated.
- Include at least one prebiotic snack - a banana, a handful of almonds, or raw veggies with hummus.
- Schedule a 5‑minute breathing break after each meal to lower stress.
- Move for 10minutes post‑lunch (walk, light stretching).
- Finish dinner at least 3hours before bedtime; keep the meal moderate in size.
- Log your meals and any gut symptoms in a simple notebook or app.
Follow this checklist for two weeks and you’ll likely notice less bloating, steadier energy, and fewer bathroom urgencies.
6. Frequently Asked Questions
How long does it take to see improvements after changing my diet?
Most people feel less gas and more regularity within 3‑7days, but full microbiome shifts can take 4‑6weeks. Consistency is key.
Are there any foods that should be avoided completely?
Highly processed foods, excess added sugars, and very high‑fat fried items can aggravate dysbiosis. Individual intolerances (e.g., lactose or gluten) should be addressed based on testing.
Can stress really affect my stomach?
Yes. Stress triggers the release of cortisol and adrenaline, which alter gut motility and increase permeability, often leading to IBS‑like symptoms.
Should I take a probiotic every day?
For most healthy adults, a daily probiotic isn’t mandatory if you eat plenty of fermented foods. Targeted use after antibiotics or during travel is more evidence‑based.
What’s the difference between a prebiotic and fiber?
All prebiotics are fibers, but not all fibers are prebiotics. Prebiotic fibers (like inulin) specifically fuel beneficial bacteria, while other fibers mainly add bulk.
Boosting gastrointestinal health isn’t a one‑size‑fits‑all prescription. It’s a blend of informed food choices, steady habits, and listening to your body’s signals. Start with the checklist, keep an eye on the warning signs, and you’ll give your gut the support it needs to keep you thriving.